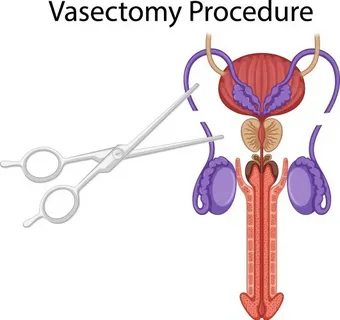
Vasectomy is widely regarded as a safe, effective, and minimally invasive method of permanent male contraception. For the vast majority of patients, the procedure results in minimal discomfort and a rapid return to normal activities. However, a small but clinically significant subset of men experience persistent pain following the procedure, often referred to as chronic post-vasectomy pain syndrome (CPVPS). While early explanations focused primarily on mechanical or obstructive causes, emerging research highlights a more complex biological phenomenon: neuroimmune crosstalk.
Understanding how the nervous system and immune system interact after vasectomy provides critical insight into why chronic pain develops in some patients and not others. This evolving perspective is reshaping diagnostic strategies, prevention efforts, and therapeutic interventions.
Understanding Chronic Post-Procedure Pain After Vasectomy
Chronic post-procedure pain is typically defined as scrotal, testicular, or pelvic pain persisting for more than three months after vasectomy and severe enough to interfere with daily activities or quality of life. The pain may be intermittent or constant, sharp or dull, and can radiate to the groin, lower abdomen, or thigh.
Historically, explanations for chronic pain after vasectomy included:
- Epididymal congestion due to sperm buildup
- Sperm granuloma formation
- Scar tissue or nerve entrapment
- Increased intraluminal pressure
While these factors can contribute, they do not fully explain the variability in pain severity or duration. Many patients with similar anatomical findings experience no pain at all, suggesting that biological signaling pathways—rather than structure alone—play a decisive role.
The Concept of Neuroimmune Crosstalk
Neuroimmune crosstalk refers to the bidirectional communication between the nervous system and the immune system. Peripheral nerves and immune cells share chemical messengers, including cytokines, chemokines, neuropeptides, and growth factors. When tissue injury occurs, such as during vasectomy, both systems are activated simultaneously.
In a normal healing response:
- Immune activation is temporary and localized
- Nerve sensitization resolves as inflammation subsides
In maladaptive responses:
- Immune signaling persists
- Nerves remain hyperexcitable
- Pain becomes chronic and disproportionate to tissue injury
This maladaptive neuroimmune interaction is increasingly recognized as a central mechanism in chronic post-surgical pain conditions, including chronic pain following vasectomy.
Immune Activation Following Vasectomy
Vasectomy disrupts the blood–testis barrier, exposing sperm antigens to the immune system. Because sperm cells develop after immune tolerance is established, they are recognized as foreign by the body once exposed.
Key immune responses include:
- Recruitment of macrophages and T lymphocytes
- Release of pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α
- Formation of antisperm antibodies
In most individuals, this immune response remains controlled. However, in susceptible patients, prolonged immune activation creates a persistent inflammatory environment within the epididymis and surrounding tissues.
Neural Sensitization and Pain Signaling
Peripheral nerves in the spermatic cord, epididymis, and scrotal skin are highly sensitive to inflammatory mediators. Cytokines released during immune activation directly interact with nociceptors (pain-sensing neurons).
This interaction leads to:
- Lowered pain thresholds
- Increased spontaneous nerve firing
- Enhanced response to mechanical or thermal stimuli
Over time, sustained immune signaling can induce peripheral sensitization, where nerves become abnormally responsive even in the absence of ongoing tissue damage.
Central Sensitization: When Pain Becomes Self-Sustaining
In some patients, persistent peripheral nerve activation triggers changes within the spinal cord and brain, a phenomenon known as central sensitization. This process amplifies pain perception and reduces the nervous system’s ability to inhibit pain signals.
Central sensitization involves:
- Increased excitatory neurotransmitters
- Reduced inhibitory pathways
- Microglial activation within the spinal cord
Once established, pain may persist independently of the original surgical site, explaining why imaging and physical examinations often appear normal in men with chronic post-vasectomy pain.
Role of Glial Cells in Neuroimmune Crosstalk
Glial cells, particularly microglia and astrocytes, play a pivotal role in neuroimmune signaling. Traditionally considered support cells, glia are now known to actively regulate pain pathways.
After vasectomy-related inflammation:
- Peripheral immune signals activate spinal microglia
- Activated glia release cytokines that enhance neuronal excitability
- Pain signaling circuits become reinforced
This glial involvement represents a critical link between immune activation and long-term neural plasticity associated with chronic pain.
Genetic and Individual Susceptibility Factors
Not all men undergoing vasectomy experience neuroimmune dysregulation. Individual susceptibility appears influenced by:
- Genetic polymorphisms affecting cytokine production
- Pre-existing inflammatory or autoimmune conditions
- Prior chronic pain disorders
- Psychological stress and anxiety
These factors may prime the immune and nervous systems toward exaggerated responses, increasing the risk of chronic pain following otherwise routine surgical interventions.
Implications for Diagnosis
Recognizing neuroimmune crosstalk shifts diagnostic emphasis away from purely anatomical causes. Traditional imaging may fail to detect functional abnormalities in nerve signaling or immune activation.
Emerging diagnostic approaches include:
- Quantitative sensory testing
- Biomarker profiling for inflammatory cytokines
- Pain phenotyping to distinguish neuropathic features
This paradigm helps clinicians identify patients whose pain is driven primarily by neuroimmune mechanisms rather than structural pathology.
Therapeutic Strategies Targeting Neuroimmune Pathways
Understanding neuroimmune crosstalk opens new avenues for treatment beyond conventional analgesics or surgical revision.
Pharmacologic Approaches
- Neuropathic pain agents (gabapentinoids, tricyclic antidepressants)
- Anti-inflammatory therapies targeting cytokine signaling
- Emerging glial modulators under investigation
Interventional Techniques
- Targeted nerve blocks to interrupt sensitized pathways
- Neuromodulation techniques for refractory cases
Multidisciplinary Management
- Cognitive-behavioral therapy to address central sensitization
- Physical therapy focused on pelvic floor and neural desensitization
- Patient education to reduce fear-driven pain amplification
Early intervention aimed at dampening maladaptive neuroimmune responses may prevent the transition from acute postoperative discomfort to chronic pain.
Prevention and Future Directions
As research advances, preventive strategies may include:
- Identifying high-risk patients preoperatively
- Optimizing surgical techniques to minimize neural injury
- Modulating early inflammatory responses after vasectomy
Future studies are exploring biomarkers and personalized medicine approaches to predict and mitigate chronic pain risk, positioning vasectomy care within a broader precision-health framework.
Conclusion
Vasectomy remains a highly effective and safe procedure for male contraception, yet chronic post-procedure pain represents a complex challenge for a minority of patients. The emerging concept of neuroimmune crosstalk provides a unifying explanation for persistent pain that cannot be attributed solely to structural abnormalities.
By understanding how immune activation and neural sensitization interact, clinicians can move beyond traditional models and adopt more targeted, patient-centered approaches to prevention, diagnosis, and treatment. Continued research into neuroimmune mechanisms promises to further reduce the burden of chronic pain and improve long-term outcomes for men undergoing vasectomy.
FAQs
1. Is chronic pain after vasectomy caused by nerve damage alone?
No. While nerve irritation can contribute, chronic pain often results from complex neuroimmune interactions involving prolonged inflammation, immune signaling, and nerve sensitization rather than direct nerve injury alone.
2. Can neuroimmune-related pain after vasectomy be treated effectively?
Yes. Although challenging, many patients benefit from targeted therapies such as neuropathic pain medications, nerve blocks, and multidisciplinary pain management approaches that address both immune and nervous system components.